Mpox_A2.PDF (423.7 KB)
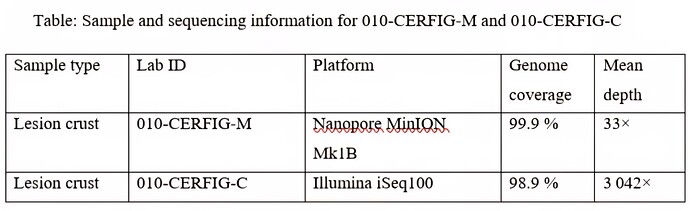
On 13 June 2025, CERFIG (Centre de Recherche et de Formation en Infectiologie de Guinée confirmed Mpox infection in a 53‑year‑old patient attending the Dermatology Department of CHU Donka, Conakry. Whole‑genome sequencing performed on crust lesion samples with Oxford Nanopore (metagenomic approach) and Illumina iSeq100 (targeted capture) recovered 99.9 % and 97.8 % of the viral genome, respectively. Phylogenetic analysis placed the virus in lineage A.2.2 of Clade IIb, clustering with the newly identified lineage from Sierra Leone designated as G.1. These findings of this lineage in Guinea illustrate the spread of this viral lineage in West Africa and underscore the need for intensified genomic surveillance, rapid case isolation, and contact tracing to control further spread in Guinea
Background
Since May 2022, the global mpox outbreak has been dominated by sub‑clade IIb, especially lineage B.1, which has caused more than 100,000 confirmed cases across 115 countries (1). Despite the decline in incidence, the outbreak remains ongoing (2). The World Health Organization declared it a Public Health Emergency of International Concern in August 2024 (3)
Mpox virus is divided into two clades (I and II), with clade II split into IIa and IIb (4). Clade IIa viruses are documented west of the Dahomey Gap in West Africa, and clade IIb regroups all the sequences from the 2022 global mpox outbreak, as well as sequences obtained from Nigeria and east of the Dahomey Gap (5).
Lineage A (within clade IIb) was first detected in southern Nigeria in 2017 and continues to drive sustained human-to-human transmission, in parallel with lineage B.1, which is now waning (6). Within lineage A, branch A.2 has expanded (sub‑lineages A.2.1 and A.2.2) and remains firmly rooted in West Africa (1).
Initially, sporadic mpox cases have been reported in the western part of West Africa, all of which are associated with a specific subclade. Surprisingly, a major outbreak attributable to clade IIb lineage A.2.2 was documented in Sierra Leone in 2025 (7). On 16 May 2025, Togo reported its first mpox cases; on‑site sequencing has already identified 22 A.2.2 genomes, suggesting rapid regional dissemination (8,9).
Guinea had reported its first mpox case in August 2024 in a 7-year-old child in Forest Guinea. The confirmed MPXV case had a Clade IIa infection linked to infection strains reported in Liberia in August 2024 and in Sierra-Leone in 2014–2017 (10).
On 13 June 2025, a case of mpox was confirmed in an adult patient in Conakry, the capital city of Guinea. Here, we report the complete genome sequence of the virus, identified as belonging to Clade IIb, lineage A.2.2. This represents the first genomic evidence of the establishment of this lineage in the country.
Methods
As part of routine surveillance for the early detection of Mpox cases, three types of samples were collected from the suspected patient admitted to the Dermatology Department of Donka National Hospital in Conakry. The three samples (whole blood, scab swab, and skin swab) were tested simultaneously. Genomic DNA was extracted using RunMei Kit (Human Runmei Gene Technology Co., Changsha, China) according to the manufacturer’s recommendations.
Two sequencing methods were used to sequence the Mpox genome. The first method, based on gDNA sequencing, involved preparing the library using the Native Barcoding Kit 24 V14 (SQK-NBD114.24) (Oxford Nanopore Technologies) and sequencing with MinION Mk1B. The second method was based on capture sequencing using the Comprehensive Viral Research Panel (Twist Biosciences, California, USA).
The reads obtained from Nanopore were analyzed using Minimap2 v2.28, Medaka v1.11.3, and bcftools v1.16 to generate the consensus with the reference genome (GenBank accession no. NC_063383.1).
The data obtained by a target enrichment standard hybridization workflow using the Twist Biosciences Comprehensive Viral Research Panel (CVRP) were analyzed on CZID (https://czid.org) and GeVarLi ( TRANSVIHMI / nfernandez / GeVarLi · GitLab ). Clade assignment was performed with Nextclade (https://clades.nextstrain.org/).
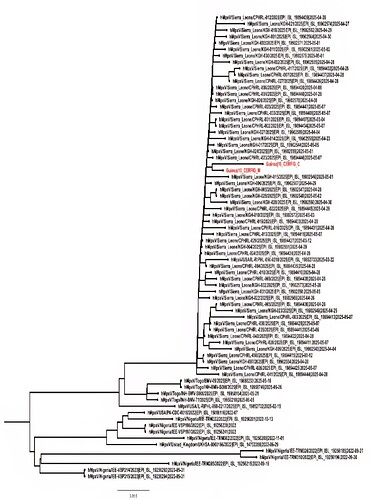
Subsequently, all good-quality sequences from lineage A.2.2 of Clade IIb available on GISAID were downloaded and aligned with MAFFT v7.525. The phylogenetic tree was based on the Maximum Likelihood model with IQ-TREE v2.3.6.
Results and discussion
Both sequencing approaches yielded complete genomes with high concordance. The Guinean virus clusters within lineage A.2.2 (Clade IIb), grouping with contemporary strains from Sierra Leone, which represent a new lineage designated G1. The close phylogenetic clustering between the Guinean genome and West African A.2.2 strains, particularly those from Sierra Leone, supports regional spread of the current alarming mpox epidemic in these countries. Targeted sampling in border districts and among travellers will be essential to reconstruct the exact trajectory of the case in Guinea.
The arrival of A.2.2 (Clade IIb) in Guinea marks a new stage in the expansion of lineage A, distinct from the B.1 wave outside Africa. High growth rates measured in Sierra Leone raise the possibility of silent spread before detection, as seen with other orthopoxviruses. Moreover, additional mpox cases have been reported since in Conakry, the capital city, illustrating that the virus started to spread also in Guinea.
This finding comes at a time when several West African countries still lack vaccine stocks, and distribution remains uneven. Integrating genomic data into vaccination strategies could help prioritise high‑risk areas.
The recently reported mpox virus strains from Togo represent another distinct cluster in the West African A.2.2 lineage, highlighting the complexity of the mpox epidemic in West Africa. Strengthen real-time sequencing: adopting high-throughput amplicon protocols to reduce the turnaround time between sampling and sequence submission is crucial for surveillance and understanding of epidemics.
Data availability
Consensus genomes are deposited on GISAID (EPI_ISL_20053179, EPI_ISL_20053180) and GenBank via Pathoplexus (accession no. OZ281549.1; OZ281547.1)
Authors Contributions
Sequencing: Abdoul Soumah, Thibaut Armel Chérif Gnimadi, Joel Balle Koivogui, Haby Diallo, Alpha Kabiné Keita Aissatou Bailo Diallo; Data analysis: Thibaut Armel Chérif Gnimadi, Validation: Alpha Kabinet Keita; Supervision: Abdoulaye Touré, Martine Peteers, Eric Delaporte, Alpha Kabinet Keita.
Acknowledgements and funding
We thank our national and international partners for their logistical support: AFROSCREEN Network, AFRICAM Project, National Hospital Donka, the Dermatology service and ANSS
Reference
1. Ndodo N, Ashcroft J, Lewandowski K, Yinka-Ogunleye A, Chukwu C, Ahmad A, et al. Distinct monkeypox virus lineages co-circulating in humans before 2022. Nat Med. 2023 Sep;29(9):2317–24.
2. CDC. Mpox. 2025 [cited 2025 Aug 2]. Mpox in the United States and Around the World: Current Situation. Available from: Mpox in the United States and Around the World: Current Situation | Mpox | CDC
3. WHO Director-General declares mpox outbreak a public health emergency of international concern [Internet]. [cited 2025 Jul 2]. Available from: WHO Director-General declares mpox outbreak a public health emergency of international concern
4. Vakaniaki EH, Kacita C, Kinganda-Lusamaki E, O’Toole Á, Wawina-Bokalanga T, Mukadi-Bamuleka D, et al. Sustained human outbreak of a new MPXV clade I lineage in eastern Democratic Republic of the Congo. Nat Med. 2024 Oct;30(10):2791–5.
5. Kinganda-Lusamaki E, Amuri-Aziza A, Fernandez-Nuñez N, Makangara-Cigolo JC, Pratt C, Vakaniaki EH, et al. Clade I mpox virus genomic diversity in the Democratic Republic of the Congo, 2018–2024: Predominance of zoonotic transmission. Cell. 2025 Jan 9;188(1):4-14.e6.
6. Otieno JR, Ruis C, Onoja AB, Kuppalli K, Hoxha A, Nitsche A, et al. Global genomic surveillance of monkeypox virus. Nat Med. 2025 Jan;31(1):342–50.
7. Mitjà O, Watson-Jones D, Choi EM, Jalloh MB, Sahr F. Clade IIb mpox outbreak in Sierra Leone. The Lancet. 2025 Jun 28;405(10497):2274–5.
8. Mpox worldwide overview [Internet]. 2025 [cited 2025 Aug 7]. Available from: Mpox worldwide overview
9. Mpox [Internet]. [cited 2025 Aug 7]. Togo reports mpox outbreak as activity escalates in West Africa. Available from: https://www.mpoxed.com/news/togo-reports-mpox-outbreak-as-activity-escalates-in-west-africa
10. Djuicy DD, Selekon B, Malaka C, Soumah A, Adjogoua E, Kadjo H, et al. Strengthening Africa’s resilience to Mpox: Preparedness and response initiatives of the Pasteur network. J Public Health Afr. 2025 Mar 31;16(1):1026.